Medicare Lift Chair Cost Calculator
Find out what you'll pay out-of-pocket for a Medicare-covered lift chair. Medicare Part B covers 80% of the approved amount for the lift mechanism only.
Enter your values and click Calculate
Note: Medicare only covers the motorized lifting mechanism that helps you stand up. Features like reclining, heat, massage, or adjustable headrests are not covered and must be paid for by you.
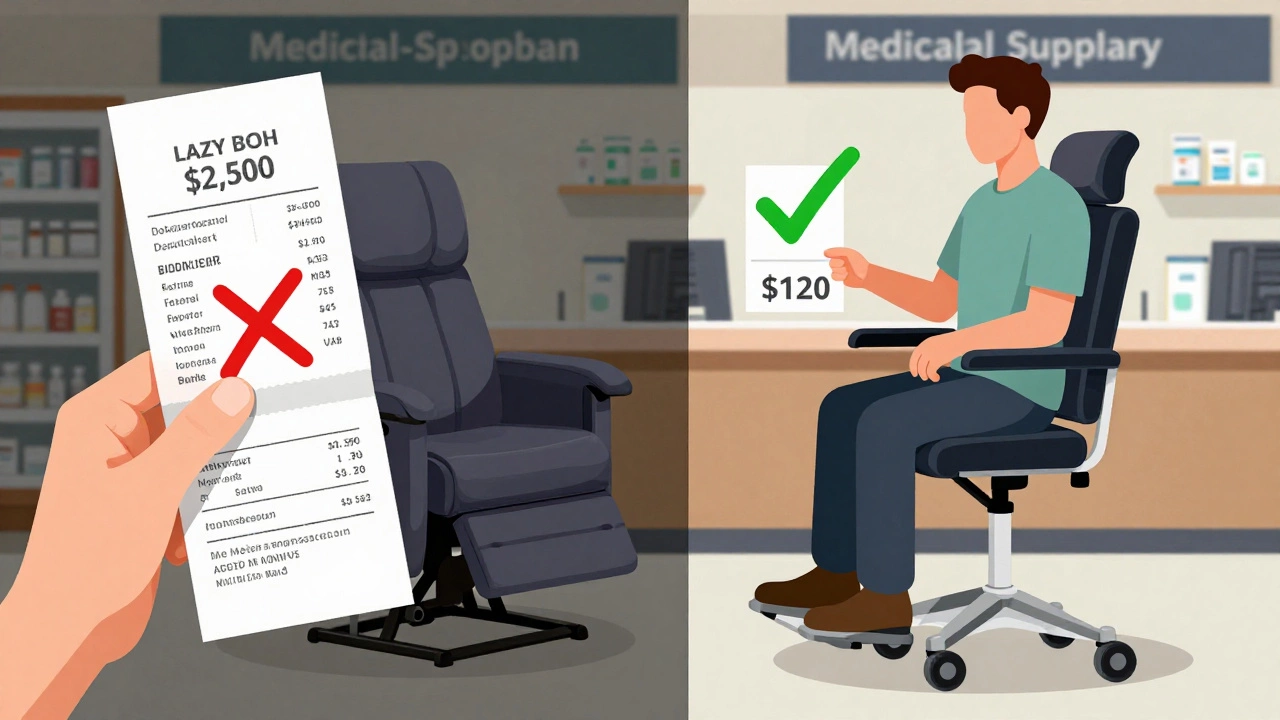
If you’re struggling to stand up from your chair, or if your knees ache every time you try to get up, you’ve probably looked into lift chairs. And if you’ve seen a Lazy Boy lift chair advertised, you might be wondering: Can Medicare pay for this? It’s a smart question - these chairs aren’t cheap, and they can make a huge difference in your daily life. But Medicare doesn’t just cover any chair that lifts. There are rules. And if you don’t follow them, you could end up paying thousands out of pocket.
Medicare doesn’t cover furniture - unless it’s medical equipment
Medicare won’t pay for a Lazy Boy lift chair because it’s a recliner. That’s not the issue. The issue is whether it meets Medicare’s definition of durable medical equipment (DME). DME must be:
- Primarily used for a medical purpose
- Generally not useful to someone who isn’t sick or injured
- Expected to last at least three years
- Used in the home
A regular Lazy Boy recliner? That’s furniture. A lift chair that helps you stand up because you have severe arthritis, muscle weakness, or mobility issues? That could be DME. The key difference isn’t the brand - it’s the function.
What makes a lift chair eligible for Medicare?
Not every lift chair qualifies. Medicare only covers models that meet specific medical criteria. To be covered, the chair must:
- Have a motorized lifting mechanism that raises the entire seat (not just the footrest)
- Be prescribed by a Medicare-enrolled doctor
- Be deemed medically necessary for your condition
- Be rented or purchased from a Medicare-approved supplier
Medicare doesn’t care if it’s a Lazy Boy, Golden Technologies, or Pride Mobility. What matters is whether the chair helps you transfer from sitting to standing safely. If you have a diagnosis like severe osteoarthritis, neuromuscular disease, or advanced heart failure that makes standing without assistance dangerous, your doctor can write a letter of medical necessity.
Medicare will only cover the lift mechanism - not the reclining function, the fabric, the heat, or the massage features. You can still get a Lazy Boy with those extras, but you’ll pay for them yourself. Think of it like this: Medicare covers the engine of the car, not the leather seats or the sound system.
How much does Medicare actually pay?
If your lift chair qualifies, Medicare Part B will cover 80% of the approved amount for the lift mechanism. You pay the other 20%, plus your Part B deductible (which is $240 in 2026). So if Medicare approves $600 for the lift feature, you pay $120 out of pocket - not $1,200 or more.
But here’s the catch: Medicare only pays based on what it considers the “reasonable” price. If you buy a $2,500 Lazy Boy lift chair, Medicare won’t pay $2,000. They’ll only pay 80% of what they approve - say, $600 - meaning you pay $1,500 for the rest. That’s why it’s critical to get a quote from a Medicare-approved supplier first. They’ll know the exact amount Medicare will cover and can give you a clear breakdown.

What if you don’t have a doctor’s prescription?
You can buy a lift chair without a prescription. But Medicare won’t pay a dime. That’s not a loophole - it’s the rule. Even if you’re 78, can’t stand without help, and your doctor says you need it, Medicare still requires a written order from your doctor before you buy.
Here’s how it works: First, schedule a visit with your primary care doctor or a specialist like a geriatrician or physical therapist. Tell them you’re having trouble standing up. They’ll examine you, check your mobility, and decide if a lift chair is medically necessary. If they agree, they’ll write a prescription and a letter explaining why. Then you take that to a Medicare-approved DME supplier. They’ll handle the paperwork and submit the claim.
Don’t skip this step. Many people buy online, pay full price, then try to get reimbursed later. Medicare won’t reimburse you after the fact. You have to go through the approved process from the start.
How to find a Medicare-approved lift chair supplier
Not every furniture store or online retailer accepts Medicare. You need a supplier that’s enrolled in Medicare as a DME provider. Here’s how to find one:
- Go to the Medicare website’s supplier directory (Medicare.gov/supplierdirectory)
- Search for “durable medical equipment” and your zip code
- Look for suppliers that list “lift chairs” under their services
- Call them and ask: “Do you work with Medicare for lift chair coverage?”
Many local medical equipment stores in towns like Birmingham, Sheffield, or Leeds have Medicare contracts. They’ll help you choose a chair that meets Medicare’s criteria and handle the claims for you. Avoid big-box stores or Amazon sellers unless they’re explicitly listed as Medicare-approved.
What about Medicaid or supplemental insurance?
If you qualify for Medicaid, you might get full coverage for your lift chair - rules vary by state. Some Medicare Advantage plans (Part C) also offer extra benefits that cover more of the cost, including features like heat and massage. Check your plan’s benefits booklet or call your insurer. You might be surprised what’s included.
Medigap (Medicare Supplement) plans can help cover your 20% coinsurance. If you have a Medigap Plan F or G, your out-of-pocket cost could drop to just the Part B deductible - or even $0, depending on your plan.
Common mistakes people make
Here’s what goes wrong most often:
- Buying online without checking Medicare approval - you’re stuck paying full price
- Assuming all lift chairs are covered - only the lifting mechanism is
- Waiting until you’re in pain to ask your doctor - get the prescription before you buy
- Choosing a chair based on looks or features - pick one that meets Medicare’s medical requirements first
- Thinking Medicare pays for installation - they don’t. You pay for setup, delivery, and assembly
One man in Derby bought a $2,200 Lazy Boy lift chair online, paid full price, then called Medicare to ask for reimbursement. They told him: “We don’t cover furniture, even if it lifts.” He ended up selling it for $800 and buying a Medicare-approved model through a local supplier. He paid $110 out of pocket.
What if Medicare denies your claim?
Denials happen - usually because the doctor didn’t provide enough documentation. If your claim is denied, you can appeal. You’ll need:
- Your doctor’s original prescription
- Medical records showing your mobility limitations
- A letter from your doctor explaining why the lift chair is necessary for your safety
Medicare gives you 120 days to file an appeal. Don’t give up. Many denials are reversed with better paperwork.
Bottom line: Yes, Medicare can cover a Lazy Boy lift chair - if you do it right
You can get a Lazy Boy lift chair covered by Medicare - but only if you treat it like medical equipment, not furniture. Start with your doctor. Get a prescription. Find a Medicare-approved supplier. Choose a model with the lift function only. Pay your 20%. And don’t pay extra for features Medicare won’t cover.
It’s not complicated. But it’s easy to get fooled by ads that say “Medicare Approved!” when they mean “We accept Medicare payments.” That’s not the same thing. Do the work upfront, and you’ll save thousands. Your knees - and your wallet - will thank you.
Can I buy a Lazy Boy lift chair on Amazon and get Medicare to pay for it?
No. Medicare only pays suppliers who are enrolled in their program. Amazon sellers are not Medicare-approved DME suppliers. Even if the product page says “Medicare Approved,” it’s misleading. You’ll pay full price and won’t be reimbursed.
Does Medicare cover the reclining feature of a lift chair?
No. Medicare only covers the motorized lifting mechanism that helps you stand up. Features like reclining, heat, massage, or adjustable headrests are considered comfort extras - you pay for those yourself.
Do I need a doctor’s note to qualify for Medicare coverage?
Yes. A written prescription and a letter of medical necessity from your Medicare-enrolled doctor are required. Without them, Medicare won’t cover the chair, even if you have a diagnosed condition.
How long does it take to get approved for Medicare coverage?
Once your doctor provides the prescription and your supplier submits the claim, approval usually takes 5-10 business days. If your case is straightforward and well-documented, you can get your chair within two weeks.
Can I rent a lift chair instead of buying one?
Yes. Medicare covers both rental and purchase of lift chairs. If you only need it temporarily - say, after hip surgery - renting may be more cost-effective. Medicare pays the same rate whether you rent or buy, so your out-of-pocket cost stays the same.


Write a comment